Whenever a resident is injured in a fall or has a pressure ulcer (bedsore), the nursing home must report it to the Centers for Medicare & Medicaid (CMS). However, there are many more incidents of falls and bedsores at nursing homes than the facilities are reporting, according to a landmark study in the Journal of the American Medical Association (JAMA).
To schedule a free case review with a nursing home negligence lawyer serving Baltimore, call Brown & Barron at (410) 698-1717 or contact us online today!
If you want more articles like this, subscribe to our free monthly newsletter by clicking here.
Most nursing homes get the bulk of their revenue from the CMS, which oversees these nursing homes to ensure quality. The CMS uses inspections and clinical assessments to help nursing homes and their staff to identify problems. A big part of the CMS’s assessment is dependent on data provided by the nursing homes themselves in what is called the Minimum Data Set (MDS).
It might seem crazy, but this means that CMS is relying on nursing homes to provide honest data on negative events that could hurt their business. The CMS has a public website called Medicare Compare to help consumers choose a nursing home. CMS uses a variety of factors to determine the nursing homes’ quality in their five-star rating system, including self-reported data. It’s no wonder that even nursing homes with terrible reputations can boast a 5-star rating on Medicare Compare.
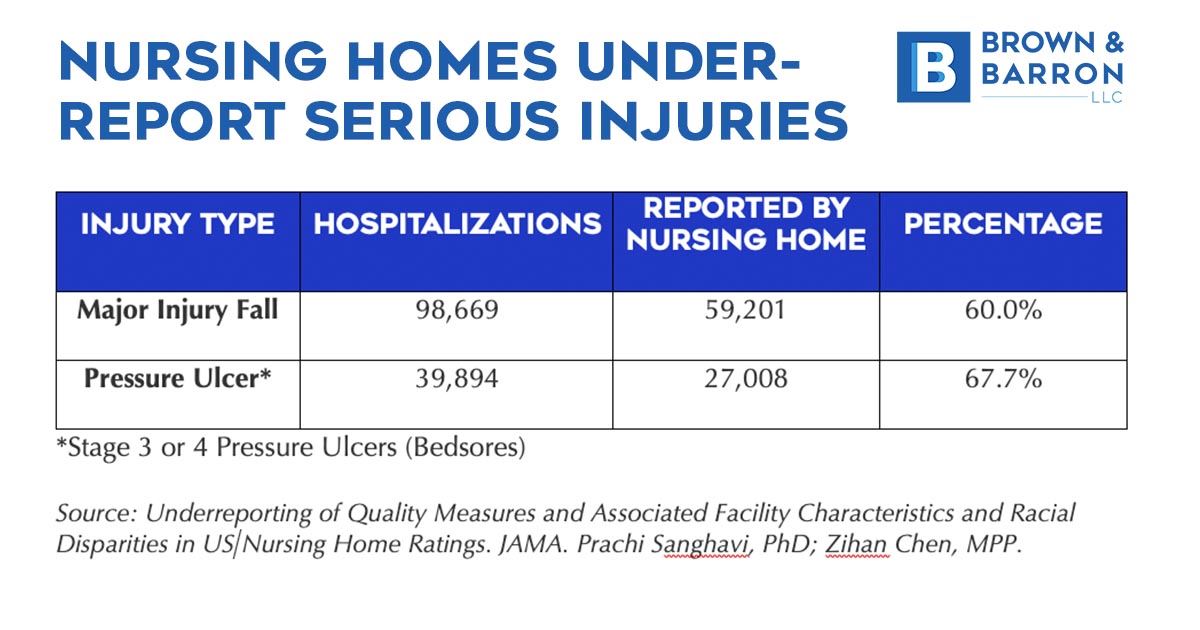
There is clearly a financial motive for the nursing home to under-report serious incidents, such as falls and pressure ulcers. The JAMA study shows just how widespread the problem is.
The Study
Authored by Prachi Sanghavi, PhD, from the Department of Public Health Sciences at the University of Chicago, the study examined 13,179 nursing homes between January 1, 2011, and December 31, 2017. The goal was to compare the nursing homes’ self-reported data on serious falls and pressure ulcers (a.k.a. bedsores) with corresponding hospital data.
The results are shocking.
“There were 98,669 major injury fall hospitalizations, of which 60.0% were reported, and 39,894 stage 3 or 4 pressure ulcer hospitalizations, of which 67.7% were reported,” according to the study.
The study also examined the data to see if there were any disparities along racial lines, reporting that “Nursing homes with more White residents had high reporting rates for major injury falls, whereas facilities with more Black residents had higher reporting rates for pressure ulcers.”
Falls in Nursing Homes
Elderly residents are more susceptible to falls and fractures at nursing home, due to age or illness. The elderly often have issues with balance, and many have mobility issues that require assistance to get around or to get out of bed or chairs. The elderly are more likely to get a fracture or worse injury, such as a traumatic brain injury from a fall at a nursing home. For the elderly, a fall can mean permanent disability or death, particularly if the hip is broken. Falls account for more than 2.8 million emergency room visits annually – and for seniors, falls are also the leading cause of fatal and non-fatal injuries, per the National Council on Aging (NCOA).
The Nursing home has a duty to conduct a comprehensive assessment of each resident's functional capabilities and to make a plan to accommodate the resident’s needs. They might need help toileting, for instance. Nursing homes are often deliberately understaffed to increase profitability. As a result, residents are often poorly attended, compelling the elderly to attempt to do things on their own that they are physically unable to do safely. Nursing homes also have a duty to keep the floors and pathways clean and clear of obstacles. Cost-cutting at nursing homes contributes to poor cleanliness, increasing the risk of falls.
Bedsores (Pressure Ulcers) at Nursing Homes
A pressure ulcer (commonly referred to as a bedsore) is a wound on the skin that occurs when pressure from body weight is applied to a spot on the body for an extended period. They are most common on the hip, back, elbows, heals, and other parts of the body without much fat for cushion. A bedsore begins as a warm spot, but over time they become infected and penetrate deeper, even reaching bone. They cause excruciating pain, and they can lead to serious long-term injuries or even death.
Bedsores are commonly the result of staying in one position in bed for too long. Healthy individuals roll in their sleep to avoid this type of extended pressure. For the very elderly, injured, or infirm (e.g., a coma), they cannot roll themselves. Bedsores can also occur to people who spend a great deal of time seated, such as those who are confined to a wheelchair.
The nursing home has a duty to assess these residents who are at risk of a pressure ulcer and to provide assistance with manual repositioning, by rolling them on regular intervals. Bedsores are referred to as a “never event” by the medical community, meaning there is never an acceptable reason that they should happen. Bedsores are always the result of negligence. Again, cost-cutting and understaffing often put nursing home staff in a no-win situation where there is not enough time in the day to meet the needs of the residents in their care. The result is certain residents are neglected for too long, leading to bedsores.
No Real Deterrent for Nursing Home Abuse & Neglect
CMS conducts random inspections and inspections when a resident or their family reports an incident, and they can levy fines for violations. However, the fines are often too low to provide much motivation for owners to take the steps necessary to avoid falls and fractures at nursing homes in Maryland or to prevent bedsores at Maryland nursing homes. The only real deterrent for nursing home ownership is the threat of a nursing home abuse or neglect lawsuit.
To schedule a free case review with a nursing home negligence lawyer serving Baltimore, call Brown & Barron at (410) 698-1717 or contact us online today!
If you want more articles like this, subscribe to our free monthly newsletter by clicking here.


